Bethany Dawson, Sarah Harris, Insider
- Women are more likely to have their chronic pain dismissed as being caused by stress and over-emotion.
- Experts say this is a structural problem caused by sexism – and the stress of this can worsen the pain.
- Doctors ignored one woman's pain disregarded and it led to her going blind.
- Visit Insider's homepage for more stories.
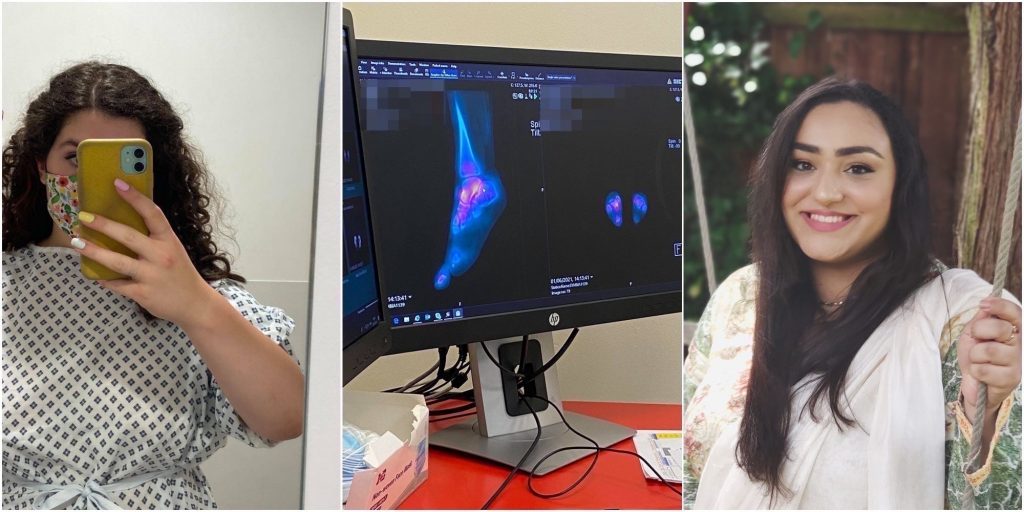
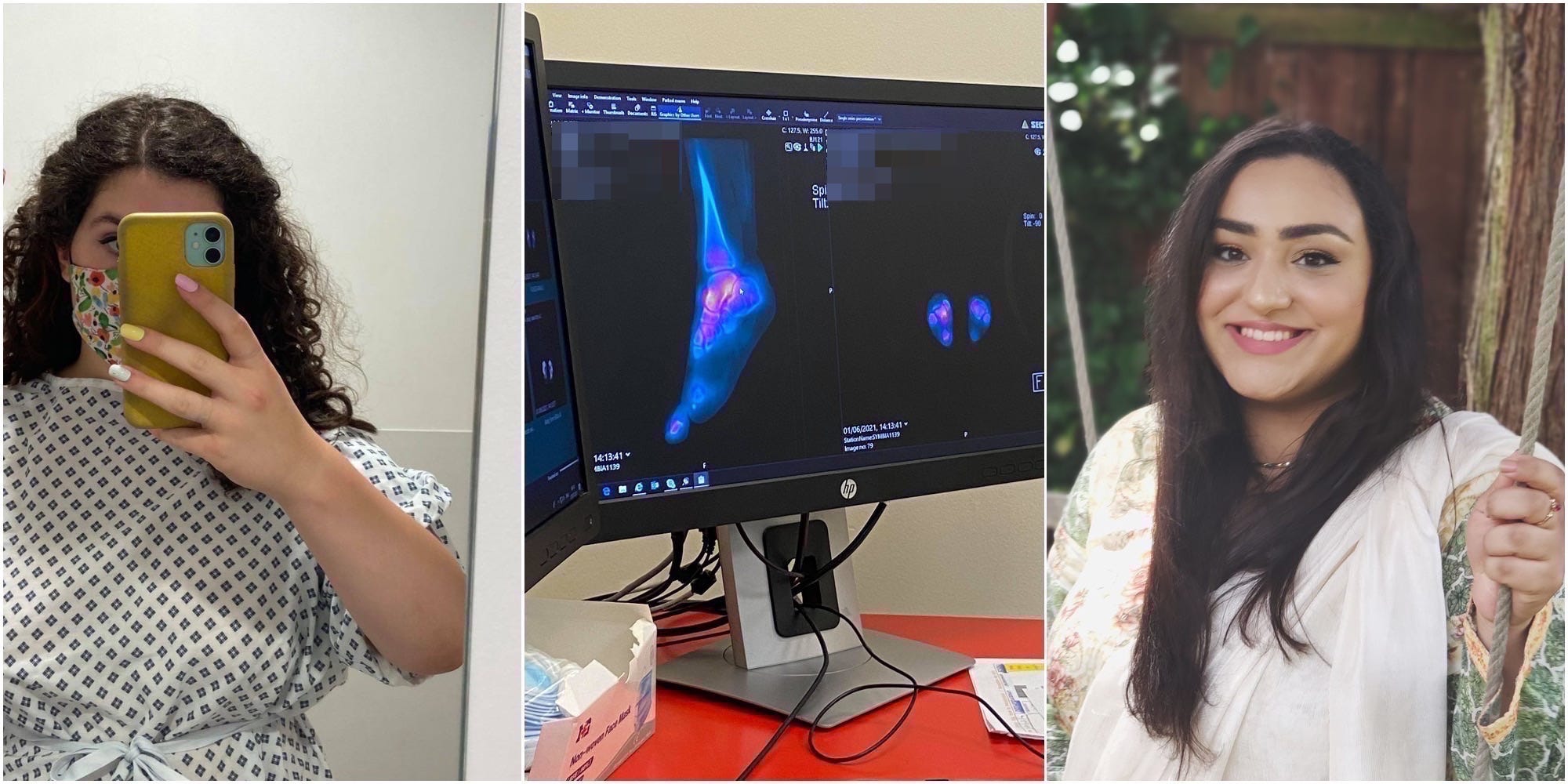
Sitting in my surgeon's office, with the clinical lighting highlighting the scans showing every inch of my painfully malformed ankles, we begin to plan the next year of my life and how it will be pivoting around major reconstructive surgery.
He explains that if my tarsal coalition – a fusion of two different joints present from birth – had been diagnosed as a child, my skeleton would have been malleable enough to remove the fusion and allow a normal foot structure to appear in its place. Now in my twenties, I'm too old to try and work to something "normal."
Instead, I have to have a complicated surgery during a global pandemic, restructuring my foot to work around a bone deformity and help me walk, albeit abnormally.
This late diagnosis is not for lack of fighting my corner or a lack of symptoms.
Rather, the cause of it lies within doctors not believing that I was suffering from any more than growing pains or a deep-rooted need for attention. I spent many hours with doctors – both in GP offices and hospitals – unable to walk properly: but no one seemed to believe that I really was in pain.
Read more: 3 ways managers can support employees living with chronic pain and fatigue
It took eight years to be heard.
This is a reality for many others too. And, unsurprisingly to those who have experienced this, it disproportionately impacts women.
Several studies have used a mechanism called GREP - Gender Role Expectations of Pain measure - to understand how the gender of a patient changes the way their experience of pain is viewed.
These studies represent why women wait longer for medical support than men. This gender-based bias could be exacerbated by the global delays in non-COVID healthcare due to the pandemic. For example, Insider's Kate Duffy recently reported on the delays in the UK health system - resulting in the life-threatening postponement of cancer treatment and canceled surgeries.
Many studies on GREP have found that women are seen as more likely, or faster to report pain and more sensitive to pain than their male counterparts.
"Women complain more than men; women are not accurate reporters of their pain; men are more stoic so that when they do complain of pain, "it's real"; and women are better able to tolerate pain or have better-coping skills than men," A landmark study on the topic - The Girl Who Cried Pain - wrote.
Another study published in May 2021 found that overall, women are perceived to be in less pain than men - even if they rated their pain at the same level as their male counterparts.
In short, women are seen as more sensitive, more dramatic, so their pain is taken to be an overreaction rather than a debilitating reality, to the extent that when men visit the emergency room with acute abdominal pain, they wait for an average of 49 minutes for painkillers. For women, it is 65 minutes.
This can have devastating outcomes.
Sarah Harris, 24, a journalist, 24, from Nottingham, in England, told Insider that she believes the invalidation of her pain led to her permanently losing 95% of her sight - something that could have been saved if the condition had been picked up earlier.
"One day, I woke up with a backache, and 24 hours later, I could barely move. Over the next few days, symptoms started to get slowly worse, but the doctors just kept telling me it was stress.
"After going to see my doctors almost every day, by chance, I happened to have a routine opticians appointment. The optician took one look at my eyes and told me I needed to go to the hospital immediately, so I did and was diagnosed with Idiopathic Intracranial Hypertension (high pressure around the brain).
"I was in hospital for a month and had lumbar punctures every few days and eventually needed emergency surgery to get a tube put in my spine. Ultimately, if my doctors had listened to me earlier on, we could have caught and prevented a lot of irreversible eye, brain, and nerve damage."

Sarah Harris
Dr Ruby Nguyen, Associate Professor in Epidemiology and Community Health at the University of Minnesota, told Insider that there are four major reasons for this pattern; clinicians misunderstanding the relationship between the psychological and the physical, poor diagnostic models, social stigma, and misogyny.
"Men are more likely to be perceived as having something concrete when it comes to pain. So, his - for example - back pain is justified because men are assumed to be more active, more labor-driven people, said Dr Nguyen.
"But society holds the stigma that women shouldn't have bodily pain because their lives are seen as less labor-intensive. So there is perceived to be no justification for a woman to have bodily pain. This is partly because society undervalues the labor that women do.
"So, when a man complains of pain, a person in their life may respond with 'go to the doctor, of course, your back hurts - you're a man, you're a strong, busy, man, why wouldn't your body hurt?' But, when a woman says that, the response is more often: 'Oh, you're just stressed out.
"What the delay in diagnosis often comes to is the need to see multiple clinicians to be heard and to get that diagnosis."
Zoe McKendree, a women's rights campaigner and domestic abuse advisor, from Brighton in southern England, spoke to Insider about her experience with this phenomenon, referred to as medical misogyny.

Zoe McKendree
"I went to see a doctor at my surgery and explained I'd been having quite intense headaches for several hours a day," She tells Insider.
"He said, "some women just get headaches" - I told him I am someone who rarely gets headaches, and he said something about "getting older," even though I was only 19.
"I continued to suffer from headaches for eight months and went to the dentist because I started to experience a lot of dental pain at the top of my mouth. The dentist told me it was because I had a severe sinus infection pushing on the roots of my teeth. The dentist prescribed me antibiotics and the pain went away within a few days. I never went back to see that GP again."
This form of invalidation often leads to a different course of treatment for women. For example, one study found that in cases of chronic pain, whilst men are more likely to get prescribed pain killers, women will be given psychotherapy - a treatment for the pain being "all in their head.'"
Dr Melinda Nicola of Murdoch University, Australia, said invalidation adds another dimension of suffering to the ignored pain.
"Pain-invalidation causes stress and anxiety. Further, evidence supports the idea that stress triggers inflammatory responses in the body, and thus could conceivably contribute to exacerbating pain."
This not to minimize the experiences that many people - regardless of gender - have with a delayed diagnosis and the invalidation of chronic pain.
For example, ankylosing spondylitis - a form of inflammatory arthritis that mainly affects people from their late teens or early twenties - takes an average of more than eight years to be diagnosed with, regardless of gender. This is due to a range of factors, Dr Nicola told Insider, including a lack of awareness of the condition and the impacts of stereotypes around what a life with arthritis looks like.
However, there is also a gendered factor in medicine that leads to women suffering longer and harder with chronic pain.
"Unfortunately, what we see here is that physicians often relate gender to how we feel about things - seeing women as more dramatic and less trustworthy when describing pain," said Dr Nguyen.